Happy Gut Bacteria, Happy Brain: The Microbiota-Gut-Brain Axis
Bacteria: Tiny Organisms Living in and on the Body
You have most likely heard about bacteria. Bacteria are very tiny creatures that are difficult to see without a microscope. They live almost everywhere. Bacteria are present in what we eat and touch. They live in and on our body. It is possible to find bacteria living in the gut or on the skin. Many millions of them inhabit our bodies. We have more bacteria than human cells in our bodies.
Normally, we associate bacteria with illness. We say that bacteria are dangerous only if they cause a disease. However, most bacteria in and on our bodies are beneficial for our health. Most of the time the body is able to control the “bad bacteria”. When the body fails to control them, it is necessary to visit a doctor. Doctors will evaluate whether we need any treatment to control bacteria or not. There are drugs that can kill bacteria or prevent them from growing. These drugs are called antibiotics. It is important to know that antibiotics kill both bad bacteria and good bacteria. So, it is important to take antibiotics only if it is really necessary, in order to keep the good bacteria alive.
Throughout our lives, we acquire bacteria. Each part of the human body has different types of bacteria. Bacteria living in the mouth are different from those ones living on the hair. Bacteria arrive in our bodies very early. For example, when we are born, we acquire our first bacteria through the contact with the skin of our mothers. Also, when we are newborns, we receive a significant number of bacteria from the food that we receive. Breast milk is one of the main sources of our first good bacteria.
Gut Microbiota: A Paradise for Bacteria in the Body
The human microbiota
Every time that we eat or drink something, it goes into the gastrointestinal tract. This is where digestion of food takes place. Digestion is a process where enzymes and acids convert food into very small fragments that can be absorbed by the gut. Enzymes are molecules that help to convert something into another thing very quickly. For example, in the gastrointestinal tract, enzymes convert pieces of food into tiny bits. Gastrointestinal cells produce these enzymes and acids. Together with gastrointestinal cells, gut bacteria help the body with food digestion. From digestion, the human body obtains nutrients, such as proteins, sugars, fats, and vitamins that the human body requires to work and grow. Bacteria also help to produce some of these nutrients. Bacteria have the capacity to convert food molecules into energy for the human body. In fact, gut bacteria produce around 10% of the energy that the body uses [2]. In the human body, the endocrine system manages the energy that the body needs. Endocrine cells produce hormones
In humans, the immune system protects the body against illness. The presence of bacteria in and on the human body helps us to have a stronger immune system. The immune system learns from bacteria how to protect the body against illness. When the body has contact with bacteria, it increases its defenses. This helps to reduce bad bacteria and to improve the environment for good bacteria, making the healthy gastrointestinal tract a paradise for the good bacteria.
The Microbiota-Gut-Brain Axis: A Connection between Gut Bacteria and the Brains
The microbiota-gut-brain (MGB) axis
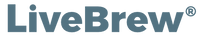
- Figure 1 - The microbiota-gut-brain (MGB) axis is a link between gut bacteria and brain.
- It is a bidirectional axis that uses the vagus nerve as main connection. This figure includes the hypothalamic-pituitary-adrenal (HPA) axis and its link with the MGB axis.
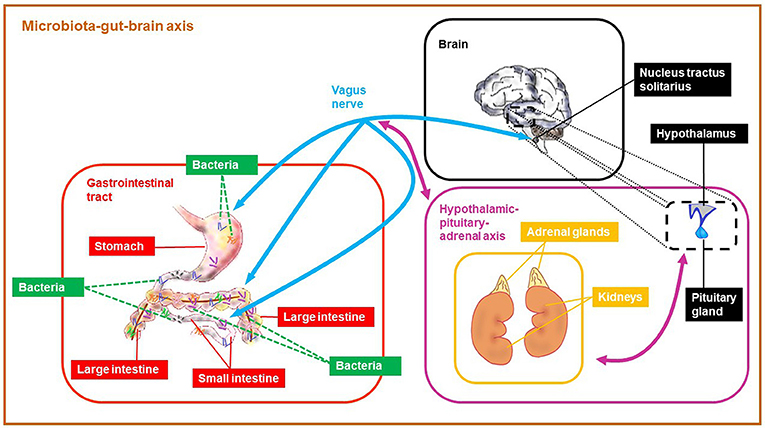
- Figure 2 - The microbiota-gut-brain (MGB) axis links the nervous system, the endocrine system, and the immune system.
- The communication between these systems is mainly possible through the vagus nerve.
The brain is part of the nervous system. It is the main control center of the body. The brain orders our muscles to move. It interprets all the things that we sense. The brain is the origin of our thoughts and mood. Scientists divide the nervous system into two subsystems: the central nervous system, which that includes the brain and spinal cord, and the peripheral nervous system, which includes all the nerve connections outside of the brain and spinal cord.
The gastrointestinal tract is connected to the brain through an important nerve called vagus nerve. The vagus nerve
is like a cable that links the heart, gastrointestinal tract and lungs to the brain. The vagus nerve links to an area of the brain called the hypothalamus
The MGB axis uses the vagus nerve as a main phone line. This communication goes in both directions, meaning that the gut microbiota can communicate with the brain through the vagus nerve, but the brain can also communicate with the gut microbiota using the same axis.
Gut Microbiota and Mood Regulation: Happy Bacteria, Happy Brain
Since the hypothalamus controls emotions, it is also an important brain structure for stress regulation. Stress is the response of the body to something that happens in our environment. Examples of daily things that induce stress are activities such as practicing sports, going to school, and sitting for an exam. In the human body, the nervous system and another axis, called the hypothalamic-pituitary-adrenal (HPA) axis
Taking Care of the Gut Microbiota: Watch What You Eat
A correct communication between the gut bacteria and the brain is important in order to have adequate mental health. The MGB axis makes this communication possible. Scientists are still trying to understand exactly how this axis works. However, it is clear that there is an association between a healthy brain and a functional MGB axis.
Diet is probably the most important strategy for maintaining a healthy MGB axis. A balanced diet, including fish, vegetables, cereals, fruits, and water is important to keep both a functional MGB axis and a good mood. The food that we consume has a direct impact on our bacteria and their home—our bodies.
Patients suffering from depression may benefit from this research on the MGB axis. These patients might be able to improve their condition by eating a healthy diet. Our habits, such as diet, definitely influence our moods, so we should take care with our diets. Eat well and be happy!
Author Contributions
JL-O, RR and TB are equally contributing authors of the original source article. JL-O wrote the first draft of this manuscript. All authors contributed to manuscript revision, read and approved the submitted version.
Funding
JL-O is supported by a Feodor Lynen Research Fellowship from the Alexander von Humboldt Foundation. The original source article was supported by the German Federal Ministry of Education and Research (Bundesministerium für Bildung und Forschung, BMBF), Research Grant No. 01EE1401B to RR and TB.
Glossary
Microbiota: ↑ Microorganisms living in a particular environment. For example, the human microbiota is the group of microorganisms living in and on the human body.
Gastrointestinal Tract: ↑ An organ that includes the mouth, esophagus, stomach, and intestines. This is where digestion of food takes place. It is the home of a large number of bacteria.
Hormones (Singular Hormone): ↑ Molecules that allow the endocrine cells to communicate with other cells of the body. They are important to manage the energy that the body needs.
Microbiota-Gut-Brain (MGB) Axis: ↑ A bidirectional connection between gut bacteria and the brain. It is a link between the nervous system, the endocrine system, and the immune system.
Vagus Nerve: ↑ A long nerve that links the heart, gastrointestinal tract, and lungs to the brain.
Hypothalamus: ↑ A brain region that controls emotions and functions like hunger and thirst.
Hypothalamic-Pituitary-Adrenal (HPA) Axis: ↑ A system that includes the hypothalamus, pituitary and adrenal glands. It links the nervous system to the endocrine system. It controls the response of our bodies to stress.
Cortisol: ↑ A hormone produced by the HPA axis that prepares the body to cope with stress—increasing blood sugar, suppressing the immune system and promoting the mobilization of fats and proteins.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
[1] ↑ Pacheco, A. R., and Sperandio, V. 2015. Enteric pathogens exploit the microbiota-generated nutritional environment of the gut. Microbiol. Spectr. 3. doi: 10.1128/microbiolspec.MBP-0001-2014
[2] ↑ Elson, C. O., and Alexander, K. L. 2015. Host-microbiota interactions in the intestine. Dig. Dis. 33:131–6. doi: 10.1159/000369534